Definitions of breathlessness?
- In this resource, we will be using the term “breathlessness” to describe the subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity.
- The experience of breathlessness “derives from interactions among multiple physiological, psychological, social, and environmental factors, and may induce secondary physiological and behavioural responses”.
- While guidelines published by the American Thoracic Society (ATS) the National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) all use the term “dyspnoea”, the definition of this symptom, as well as the terms that should be used to assess its occurrence, severity, distress, and impact are not standardized. Of note, patients use a variety of words to describe dyspnoea (e.g., “shortness of breath”, “difficulty breathing”, “chest tightness”, “air hunger”. This lack of a standardised nomenclature is a significant limitation to be able to make comparisons across studies and develop a comprehensive symptom assessment instrument.
- It is important to define breathlessness is a symptom rather than a clinical sign
It must generally be distinguished from signs that clinicians typically invoke as evidence of respiratory distress, such as tachypnoea, use of accessory muscles, and intercostal retractions.
- Whilst previously thought to be related to hypoxia or work of breathing, subsequent research has demonstrated that breathlessness arises as a complex interaction among multiple physiological, psychological, social, and environmental factors.
- Specific physiological processes may be linked to corresponding sensory descriptors, the best characterized of which are:
- Sensations of work or effort
- Sensory–perceptual mechanisms underlying sensations of work or effort in breathing are similar to those underlying similar sensations in exercising muscle.
- Tightness
- Tightness is relatively specific to stimulation of airway receptors in conjunction with bronchoconstriction.
- Air hunger/unsatisfied inspiration
- Intensity of air hunger/unsatisfied inspiration is magnified by imbalances among inspiratory drive, efferent activation (outgoing motor command from the brain), and feedback from afferent receptors throughout the respiratory system.[1]
- Acute vs chronic
- Sensations of work or effort
Why is breathlessness important?
- It is estimated that up to a quarter of the general population and half of severely ill patients are affected by breathlessness.[1]
- In patients with chronic obstructive pulmonary disease (COPD), it has been shown to be a better predictor of mortality than forced expiratory volume in 1 s. In patients with heart disease it is a better predictor of mortality than angina. Breathlessness is also associated with decreased functional status and worse psychological health in older individuals living at home. [4]
- Despite its tremendous burden, breathlessness is often underestimated by clinicians. For example, while clinicians reported that less than 30% of patients with lung cancer experienced moderate to severe breathlessness, over 50% of their patients reported the occurrence of this symptom. [5]
What causes breathlessness?
- Sensory Afferent Information: Sensory afferent sources for respiratory sensation include traditionally defined sensory afferents and information from respiratory motor areas of the brain. The latter can send an ascending copy of their descending motor activity to perceptual areas, known as corollary discharge. This corollary discharge has been well described in the limb motor control literature. The respiratory motor system is unusual in having both automatic (brainstem) and voluntary (cortical) sources of motor command; corollary discharge from these different sources probably gives rise to different sensations.
- Qualities of breathlessness
- Work/effort: This was once believed to be responsible for all breathlessness, but this idea has been disproved. However, an uncomfortable sense of respiratory work and effort is commonly reported by patients with conditions like asthma and COPD. Respiratory muscle afferents project to the cerebral cortex, and subjects report sensations localized to respiratory muscles when the work of breathing is high. Perceptions of work and effort probably arise through some combination of respiratory muscle afferents and perceived cortical motor command or corollary discharge.
- Tightness: Commonly experienced during bronchoconstriction, tightness is often the dominant experience in the early stages of an asthma attack. As airway narrowing worsens, patients also report work/effort and air hunger/unsatisfied inspiration. Bronchoconstriction gives rise to both a sense of tightness and added physical work of breathing; however, blocking pulmonary afferents can diminish tightness.
- Air hunger/unsatisfied inspiration: This perception of not getting enough air can be induced experimentally by increasing inspiratory drive, especially if the capacity to satisfy the increased ventilatory demand is limited. As the demand for ventilation exceeds the capacity to provide it, a state of imbalance develops between the motor drive to breathe, as sensed via corollary discharge, and afferent feedback from mechanoreceptors of the respiratory system. This becomes increasingly unpleasant and distressing.
- These sensations can be intensified by stimuli that increase spontaneous ventilatory drive, such as hypoxia, hypercapnia, acidosis, and signals arising from exercise-related drive. The interplay among neurophysiological mechanisms is complex and not fully captured by any single term.
- Neuroimaging techniques like Positron Emission Tomography (PET) and Functional Magnetic Resonance Imaging (fMRI) have been used to study neural activation from changes in cerebral blood flow. These techniques have identified specific brain regions activated during laboratory-generated breathlessness in healthy subjects; however, the design, analysis, and interpretation of these studies are complex. Inferring breathlessness-related activity can be challenging due to factors such as acute hypercapnia altering cerebral blood flow independently of neural activation. Despite these complexities, a core pattern has emerged: breathlessness activates cortico-limbic structures that also subserve interoceptive awareness of homeostatic threats such as thirst, hunger, or pain.
- Several studies have reported activations in the right anterior insular cortex and cerebellum when inducing respiratory discomfort in healthy participants. However, the cerebral regions activated in these initial breathlessness imaging studies were similar to those seen with somatic pain, except for the amygdala, which is activated in visceral pain.
- There is also an interest in the cerebral correlates of the interaction between emotion and respiratory sensation. For instance, increased insular activation has been noted in patients with idiopathic hyperventilation compared with normal, healthy control subjects exposed to repeated transient inspiratory occlusions. Conversely, decreased insular activation has been found after opiate administration, in patients with obstructive sleep apnoea exposed to inspiratory loads, and in patients with congenital central hypoventilation.
- A two-stage model by Lansing et al. proposes that immediate unpleasantness triggers withdrawal, followed by emotional responses leading to long-term adaptations. Studies suggest a complex interplay between the intensity of the sensation and its perceived unpleasantness. While the perceptual intensity may be lower than unpleasantness in some cases, negative emotions can amplify unpleasantness.
- Furthermore, the environment and emotional state significantly influence breathlessness perception. Positive affect reduces breathlessness, while negative affect worsens it. Interestingly, manipulating emotions seems to impact unpleasantness rather than the intensity of the sensation itself.
- Clinical observations support these findings. Patients with high anxiety/depression experience worse breathlessness and prognosis, while breathlessness itself can exacerbate anxiety and depression.[4]
- Opioids are thought to reduce breathlessness, as they alleviate the discomfort associated with air hunger, but not the discomfort of work or effort. Their mechanism of action likely involves a reduction in spontaneous respiratory drive and modulation of cortical activity, similar to their role in pain management.
- Decreased insular activation in response to breath-holding has been observed following opioid administration, suggesting that imaging studies could help identify the specific sites of opioid action.
- Research has also explored the potential role of endogenous opioids in modulating breathlessness. Several studies have compared the effects of the opioid antagonist naloxone and placebo in both healthy subjects and patients with COPD using a randomized, double-blind, crossover design. The results of these studies have been mixed, with some showing an increase in both ventilation rate and perceived difficulty breathing with naloxone compared to placebo, and others showing no effect.
- However, interpretation and comparisons between these studies are complicated by methodological differences, such as sample composition, physiological stimuli, endpoints, naloxone dose, and how breathlessness was measured.
- In summary, the neurophysiological mechanisms of breathlessness involve a complex interplay of sensory afferents, motor commands, and perceptual areas in the brain, leading to distinct sensations of work/effort, tightness, and air hunger. These sensations can be intensified by various physiological conditions and are commonly reported in patients with respiratory diseases. However, our understanding of these mechanisms is still evolving.[1]
- Further reading: [4]
Aetiology
- The most common causes of acute breathlessness in patients attending the accident and emergency department are:
- Asthma
- COPD
- Heart failure
- Pneumonia (or other infection)[6]
- The prevalence of chronic breathlessness is difficult to ascertain, due to studies reporting both acute and chronic breathlessness, but it has been reported to affect between 9% and 59% of the general population. A higher prevalence of chronic breathlessness has been reported in individuals over 70 years of age, with breathlessness in these patients being associated with worsening functional decline and increased five year mortality. Additionally, the aetiology of chronic breathlessness is multifactorial in approximately one third of cases, with common co-existing conditions contributing to symptomatology. [2]
- Five main aetiological categories account for most cases of chronic breathlessness (duration >1 month):
- Pulmonary disease
- Cardiovascular disease
- Respiratory muscle dysfunction
- Psychogenic breathlessness
- Deconditioning/obesity.[7]
Cancer related breathlessness
- Weighted grand mean prevalence of breathlessness in patients with advanced cancer was 58%. [8]
- In advanced cancer the prevalence of episodic breathlessness has been recorded at 70.9%. [8]
- Further factors increasing the rate of breathlessness include thoracic malignancies, with advanced stages of disease, and in the last weeks of life.
- Reversible causes of breathlessness in cancer (Management Disease Oriented Reversibility)
Impact of breathlessness
-
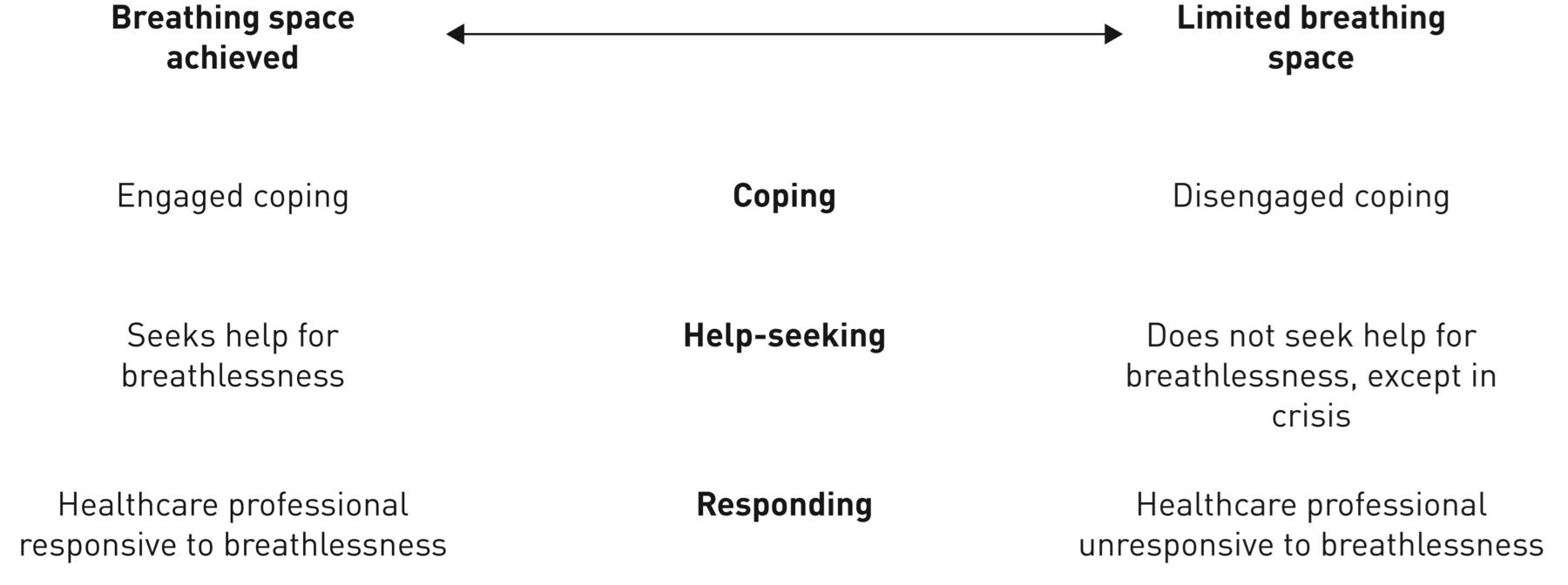
- Systematic review of the qualitative research on the experience of being breathless found four main themes:
- Widespread effects of breathlessness
- Coping
- Help-seeking behaviour
- Clinician’s response to the symptom of breathlessness
- The authors combined these themes to introduce the concept of “breathing space”, to show how engaged coping and appropriate help-seeking (patient) and attention to symptom (clinician) helps maximise the patient’s quality of living with breathlessness.[9]
- Systematic review of the qualitative research on the experience of being breathless found four main themes:
Chronic breathlessness syndrome
- Like pain, breathlessness can resist treatment of the identified underlying condition(s), but nonetheless can itself be a primary target of medical management, irrespective of the causative disease.
- Breathlessness leads to serious limitations and distress for patients and their families, and negatively impacts on emotional function, with resulting low mood and poor quality of life often accompanied by episodes of more intense breathlessness and panic.
- “The experience of breathlessness that persists despite optimal treatment of the underlying pathophysiology and results in disability for the patient”[3]
- An observational study of almost 50,000 patients with COPD in the UK revealed that a third of those with stage disease described moderate to severe breathlessness, whereas over 20% of those with stage 4 disease did not have clinically significant breathlessness. In a recent controlled trial, bronchoscopic lung volume reduction significantly improved FEV1 by 25%,without relief of breathlessness. The inconsistent relationship between pathology and breathlessness perception explains why optimising disease management alone does not guarantee good symptom control. This discrepancy has led to several terms suggesting exaggerated symptom perception, such as ‘disproportionate breathlessness’, ‘breathlessness out of keeping with pathology’ and ‘medically unexplained breathlessness’. It is apparent that there must be factors influencing breathlessness beyond that expected due to the underlying disease.[10]
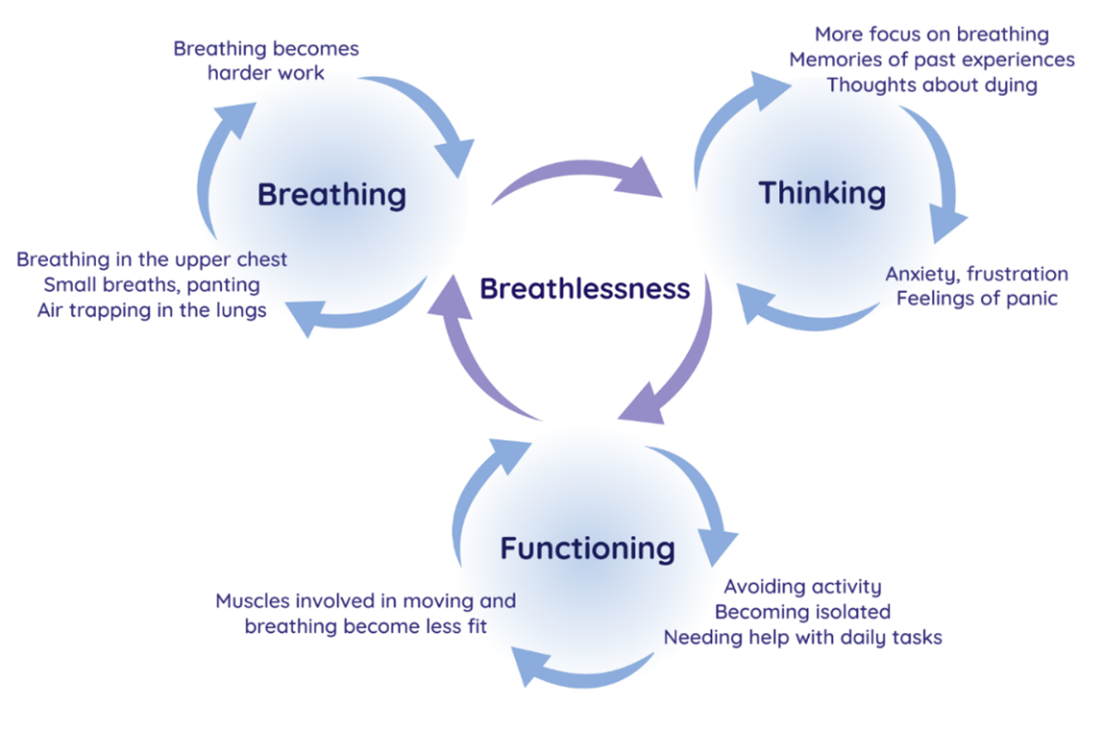
- Breathing, Thinking, Functioning Model[10]
What does being breathless feel like?
-
- Professor Miriam Johnson and Dr Ann Hutchinson of the Wolfson Institute organised an exhibition together with people with chronic breathlessness to explore the experience of living with breathlessness in Hull.
- Images were created collaboratively by visual artist Anna Bean and people living with breathlessness to describe their lived experience.
- Dr Rob MacKay, who was Reader in Music at the University of Hull during the project (and now Senior Lecturer in Composition at Newcastle University) facilitated discussions with the participants, explored their personal experiences of living with breathlessness and the strategies they used to cope with it to create a cohesive narrative that captured the multifaceted nature of their shared experiences.
To request to host the exhibition please email Dr Ann Hutchinson.
- Kate Binnie is a music therapist, yoga and mindfulness teacher with an Msc in Palliative Care and a special interest in the relationship between breath and emotion regulation, and how this can be used clinically in the management of refractory breathlessness across advanced disease.
- “Working as a therapist with people towards the end of their lives, and with a particular interest in the power of breath regulation as a tool for emotion regulation and symptom control, I started making this ‘breath-voice collage’ by recording an ‘anchor’ breath, which would act as a metronome throughout the piece. This was the sound of a heartbeat timed to a ‘coherent’ breath. This breath, commonly used by meditators and yoga practitioners, is timed at five breaths per minute, and has been shown to help people recover from trauma and anxiety disorders, and to relieve physical and psychological pain (see Brown & Gerberg 2012) and I often use this in therapy. I then interwove recordings I had saved on my iphone over the years…. my children as babies, their sleeping breaths, an old recording of my partner and I singing our child to sleep. I also recorded the breathing of a patient with chronic obstructive pulmonary disease (COPD) and his words, describing how he felt about his loss of breath. Lastly, I used a recording of my father’s breathing during his last days in the hospice. During that time, the sound of his breath was extremely important, precious and fragile because we knew it would end. In the liminal phase between life and death I sang to him the songs he loved. The Skye Boat Song was one of his favourites….”
- Developed by the Cambridge Breathlessness Intervention Service (CBIS) in 2012 as an educational tool for healthcare professionals to explain the mechanisms of worsening symptoms in patients with chronic breathlessness and to aid choice of non-pharmacological interventions with which to help them, this model uses a “vicious flower” maintenance model adapted from cognitive behavioural therapy alongside well-evidenced features in each domain. For example, attempting to avoid the perception of breathlessness by reducing activity leads to deconditioning which in turns worsens breathlessness! This model both aims to explain the way in which breathlessness perpetuates and worsens, but also provides a structure and rationale for its management—through aiming to turn vicious cycles into ‘cycles of improvement’.
- Management Non-pharmacological
Bibliography
Please click on the links below to be taken to the individual references:
[7] Kuzniar TJ. Assessment of dyspnoea. BMJ Best Practice 2024. (accessed July 15, 2024).