Learn more about how we’re uniting medical professionals dedicated to providing exceptional palliative care for those facing life-limiting illnesses.
Our membership and work are driven and bound by a contract of shared values through our Leadership PACTE. We strive to be:
Clinically Excellent
– Expert in assessing and managing the clinical aspects of patients’ suffering.
– Skilled in helping individual patients and those important to them to engage with their unique circumstances and the uncertainty, complexity and finely balanced interests and decisions that are part of their life’s conclusion.
– Professionally objective and tempered with compassion that supports and empowers those in receipt of our care.
Person-centred
– Focussed on patients’ goals and concerns above and beyond their disease(s) alone, including the related needs of those important to them.
Academically Excellent
– Inquisitive, evidence-led and willing to challenge and advocate where fresh evidence and experience are counter to or challenge established opinion or the status quo.
– Advocates for and, where feasible, participators in relevant research into contentious and neglected areas of palliative care.
– Skilled in ethical analysis, complex problem solving and shared decision-making.
Leaders
– Bold, innovative and boundary-breaking while accepting the complexity of the area in which we serve.
– Active participators in professional and societal debate surround health, care, well-being, illness, death and dying.
Transparent and Collaborative
– Able to embrace the multi-professional practice.
– Collegiate and accountable within multi-disciplinary teams.
– Willing to assist colleagues with their professional challenges around death and dying and its personal impact.
– Collaborate with other specialist organisations and disciplines.
– Open to change and scrutiny.
– Progressive and willing to engage with the opinions and perspectives of others.
Our Vision
We seek to create a future where all people with life-limiting and life-threatening illnesses live as well as possible for the duration of their natural lives and in which no one needs to die in distress or discomfort for lack of access to the best palliative care.
Our Mission
We will promote professional development and societal debate and advocate with and on behalf of all those who are involved in Palliative Medicine in order to promote, facilitate, advance and develop excellence for the benefit of every individual patient and those important to them.
APM Annual General Meeting Papers
Here you can find papers pertaining to the most recent APM AGM papers and minutes. Should you have any questions regarding these resources, don’t hesitate to contact Compleat Secretariat.
2025
What is Palliative Medicine?
Palliative Medicine provides clinical leadership, care and support to prevent and relieve suffering for people with life-limiting and life-threatening illnesses.
- Its diagnostic and therapeutic priorities focus on meeting every individual patient’s goals through shared decision-making with them and those important to them
- It is practised both as part of multi-disciplinary palliative care teams and in partnership with other relevant specialities to deliver individualised, holistic care
- It is a medical speciality recognised by the respective nations’ Royal Colleges of Physicians
Palliative Medicine’s specific expertise is in:
- Assessing and managing physical, psychological and spiritual symptoms and mitigating distress
- Clinical analysis of and decision-making in complex scenarios, such as when a patient’s clinical needs, preferences and interests are finely balanced and may require the skilled application of relevant ethical and legal guidance
- Skilled communication about and coordination of care, especially at disease transitions and boundaries between care settings
- Working with partners, colleagues and organisations across multiple sectors to provide excellent multi-disciplinary care for patients and those important to them
- Care and support to those important to the patient, including facilitating their bereavement care
What is Palliative Care
- Palliative care is active, total care of patients whose disease is not responsive to curative treatment
- The control of pain and other symptoms and of psychological, social and spiritual problems is paramount
- The goal is to achieve the best possible quality of life for patients and their families
- Priorities focus on meeting every individual’s goals to deliver individualised, holistic care
Aims of Palliative Care
- Affirm life and regard dying as a normal process
- Relieve pain and other distressing symptoms
- Integrate psychological and spiritual aspects of patient care
- Help patients live as actively as possible until death
- Provide a support system to help families cope during the illness and in their bereavement
APM
The Association for Palliative Medicine of Great Britain and Ireland (APM) is one of the world’s largest representative bodies of medical/health care professionals practising or interested in Palliative Medicine. It was formed in 1986 and has a growing membership of over 1,300. It represents healthcare professionals of all grades working in or interested in specialist palliative care, whether in hospices, hospitals or the community.
Getting into Palliative Medicine
Why choose Palliative Medicine as a career?
- The work is more patient-centred, I find, and I get to give the kind of care to patients that I myself would want …
- It’s a young speciality that’s developing fast … we link well with other specialities that deal with chronic conditions
- It’s got it all: research, management, education, and service development … you will find your niche
How do I improve my chances of getting into Palliative Medicine?
- Check the Person Specification paperwork available. This is available through the HEE Specialty Training Website
- Check the ST4 Person-Specification paperwork available. This is available through the RCP Application Website.
- Measure yourself and your CV against the ‘Essential’ and ‘Desirable’ criteria.
- Market yourself and your interest in the speciality.
It is harder, nowadays, to gain a standalone training post in a hospice, which would give you the ideal experience of what a career in palliative Medicine involves and whether you really can commit yourself to it. Nevertheless, look for other opportunities where you can link up with specialists in palliative Medicine. For example, as a post-foundation doctor, try to organise a ‘taster session’ during your training with a local hospice. Why not enter prizes organised by the Association of Palliative Medicine? There are essay prizes for undergraduates or audit prizes for junior doctors.
Note the application deadlines, and do not give up!
If you are unsuccessful after both rounds of recruitment, seek advice from your deanery’s training programme director for palliative Medicine. If your heart is set on the speciality, consider a non-training grade hospice post, which would give you valuable clinical experience in the speciality as well as demonstrate your commitment.
How do I apply?
Applications (Round One) usually open in November for a start date between August to December. More information regarding this is available on the PHS Recruitment website.
The application form can take many hours to complete, so don’t leave it until the last minute!
Once the application form has been reviewed, candidates will be short-listed for an interview based on scoring the application form. The interview has four interview question sections lasting 5-8 minutes each.
You will be marked in each of these four question areas, with a fifth mark being given for your communication and reflection skills in the ethical scenario. The entire interview will last around 30 minutes.
The four questions are:
Question 1: Suitability and Commitment: This will give you an opportunity to expand on your application form. This station will last approximately 5 minutes.
Question 2: Medical Registrar Suitability: This will explore the non-clinical parts of being a medical registrar, including managing an unselected take and managing an MDT. This will last approximately 5 minutes.
Question 3: Professionalism and Governance: This will be a discussion on professionalism and governance. The interviews will give you a single sentence or short question to prompt discussion. This assessment will be underpinned by GMC Good Medical Practice.
Question 4: Ethical / Communication Scenario: You will be scored on your skills in handling an ethical scenario and will receive another mark for your communication and reflection skills. The ethical scenario will be a hypothetical situation given to you in a written format. You will be given 5 minutes to prepare and then will have 8 minutes to perform a role-play. You will then be given 2 minutes at the end to reflect on your communication skills at the end of the role play.
The panellists were looking for ‘good all-rounders’ who showed genuine enthusiasm for and commitment to high-quality palliative care
Top tips for success!
- Have a look at the short-listing criteria
Small adjustments to your current audit or teaching projects may radically alter your short-listing score when you come to apply.
- Get the experience of working as part of a Palliative Care Team.
This is helpful (though not essential) to be able to deal with clinical and ethical scenarios at the interview – if you haven’t had the opportunity to work in palliative care, try to organise a “Taster” week.
- Attend a palliative care course and/or conference
A great way to familiarise oneself with “hot topics” in palliative care research and practice. Ask your local palliative care team about upcoming events.
- Practice your interview technique
Run through likely questions or scenarios with a friend or colleague and consider attending a communication skills course.
- Set aside time to prepare your portfolio
You will need to provide evidence of all achievements mentioned on the application form, and there is strict guidance regarding how to present it.
APM Annual General Meeting Papers
Here you can find papers pertaining to the most recent APM AGM papers and minutes. Should you have any questions regarding these resources, don’t hesitate to contact Compleat Secretariat.
2025
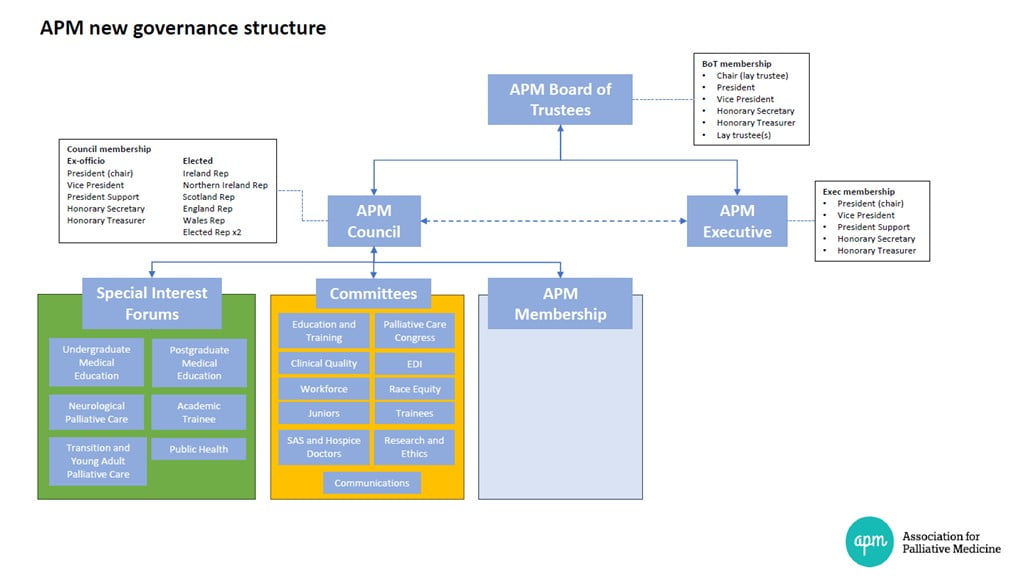
The Association.
The Association for Palliative Medicine of Great Britain and Ireland (APM) is one of the world’s largest representative bodies of medical/healthcare professionals practising or interested in palliative care, with a growing membership of over 1,300. We welcome international members.
- Full and Associate membership is open to both doctors and other medical professionals practising or interested in palliative Medicine
- Student membership is open to undergraduate medical students
We work in strategic alliance with those who can contribute to achieving our vision, supporting our values and delivering our aims.
The APM represent you, our members, to ensure that your voice is heard and that you are represented in all areas relative to Palliative Medicine practice (e.g. legal, political, training, economic and workforce), as well as many other issues, including continually changing topical national debates and essential matters such as assisted dying, palliative care funding, clinical nutrition and hydration, assisted ventilation and Palliative Medicine Training.
Want to see APM’s objectives and strategies?
Careers in Palliative Care – Introduction
Palliative Medicine is a rewarding career that allows you to support patients and families at vulnerable times. There are opportunities for complex problem-solving, challenging communication and fascinating ethical dilemmas. Good palliative care requires multi-professional teams and interactions with various hospital and community colleagues. Palliative Medicine specialist training happens in hospitals, hospices and the community.
Training full-time in a numbered post takes four years to gain a certificate of completion (CCT) in Palliative Medicine. Since 2022 Palliative Medicine has been dual accredited with General Internal Medicine, meaning that one year out of the four years of specialist training will be spent in acute Medicine.
The RCP census shows that Palliative Medicine is the 11th largest medical speciality, with around 700 consultants in the UK. Trainee numbers in Palliative Medicine are increasing. Approximately 48% of consultants work less than full-time, and a similar number of trainees choose to train flexibly.
About a third of consultant jobs are joint NHS/third sector, reflecting the fact that there are options to work across settings and organisations. Speciality trainees rate their training highly in the GMC trainees’ annual survey.
The transformation of the NHS following the COVID-19 pandemic will require increased speciality training numbers. Increased numbers of medical student placements have already been announced. This will allow an expansion of the palliative medicine workforce with roles required in all settings.
If you would like to learn more, visit our ‘About Palliative Care‘ page
For more information, please see the following resources:
Palliative medicine | Health Careers

