12 hours over course of IM training, including 4 hours in the last year. Recognised that this can be difficult to get, but SIM lead posts and further courses are being developed.
Frequently Asked Questions: Preparing for ARCP (new Palliative Medicine curriculum)

Learn more about what motivates us to advocate for our members
Uploading course certificates to personal library and reflection.
Human factors training need to be done in a Simulation setting. Advanced communication skills training also counts for human factors training (but not the public health in palliative care course).
Trainees need to keep their ALS in date during all higher specialty training.
Trainees are expected to use their study leave allowance for both Pall Med and IM focused study, including regional study days, Deanery-approved study days, courses approved for CPD and simulation (grand rounds etc. are not included).. Approximately 25% of CPD should be IM-focused: the IM ARCP decision aid IM states that 75hrs of IM CPD across training is required.
Trainees will still need an IM educational supervisor report for IM, even in a year where they have not done a formal block of IM (but will have attended KIT days.) In such a year, trainees are not expected to have any MCRs from IM (unless they have worked with one consultant consistently for their IM KIT), but they will be able to evidence their IM capability in several ways, e.g.:
- Reflections on attendance at IM KIT, e.g., specialist clinics, SDEC/ ambulatory/ AMU session, involvement in acute unselected take (AUT)
- Reflection on participation in IM-related CPD or Simulation
- IM-focussed supervised learning events from Palliative Medicine, e.g., MDT-working, complex communication, discharge planning
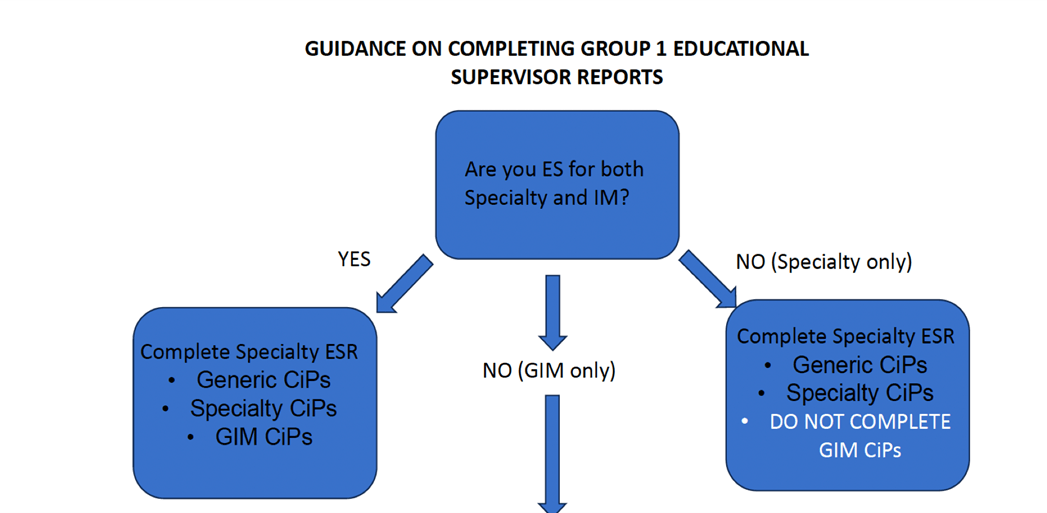
Trainees are expected to have educational supervisors for both IM and Palliative Medicine. However, in some regions this is not possible as there isn’t the capacity amongst IM-trained consultants. Please see the chart below for who completes the ESRs depending on whether there are separate IM and Pall Med supervisors.
If a Pall Med ES is completing the IM and PM ESR, they should use information in the portfolio to support entrustment decisions, including the IM MCRs, the MSF (IM respondents), IM-focused SLEs and reflections. Where possible, direct communication with the IM clinical supervisor by phone or email can help to address any inconsistencies in feedback and support the final ESR.
Where a trainee has a separate IM supervisor, they will complete the ESR. The Pall Med ESR can feed into the IM component of the ESR in areas where they have direct knowledge, e.g., CiP8 and components of other CiPs, e.g., discharge planning/ MDT working. However, the IM CiPs should be completed by the IM ES.
In the unlikely event that what the Pall Med and IM ESs give very different assessments, this will be reviewed by the ARCP panel. Trainee self-assesses their entrustment levels prior to finalising the ESR, allowing any disparities to be visible to supervisors, allowing them to discuss and agree any revisions prior to completion of the final ESRs. If disparities persist, further clarification might be sought by the ARCP panel from the supervisors, or the panel may feel able to make a judgement on progress based on the evidence in the portfolio. It is recognised that trainee progress across all of the CiPs may vary and will not necessarily impact on progression.
The Pall Med decision aid asks for a summary of clinical activity ‘Hospital, palliative care inpatient/hospice and community: number and range of patients seen in different settings to evidence sampling across range of curriculum’.
Trainees are not expected to log every single contact, but to be able to describe and evidence the breadth of their Pall Med clinical activity in different settings. Therefore, reflections on the range of patients managed in an average week in a hospital team, on a hospice inpatient unit, in outpatients, via community MDTs or domiciliary visits and on call are all useful. It is also helpful to be able to reflections on more specialist training, e.g., ward rounds or clinics with acute oncology or pain teams; or experience of working with patients with dementia, frailty, multiple long-term conditions and organ failure. Any evidence uploaded to the portfolio supports trainee and ES to reach entrustment decisions for the specialty CiPs.
There is a minimum requirement for the number of patients seen on AUT and on non-Palliative Medicine clinics attended (see IM decision aid.)
These are not yet available in the Pall Med e-portfolio. Once available, they will make preparation for ESR/ ARCP easier. The form will auto-populate. The ESR remains the important evidence to support ARCP.
Where a trainee has done different training blocks over a training year, the MSF respondents will be linked to the relevant block and it is not possible to create one summary report, without asking the JRCPTB e-portfolio team to manually move responses.
If trainees have done a block of IM that training year, MSF responses should be from both IM and Pall Med (a minimum of 4 responses should come from IM.) ESs can either review the two sets of responses to comment in the ESR or, if they have time, as the JRCPTB team to amalgamate.
The issue has been escalated to the e-portfolio team and we hope will be addressed!
The Palliative Medicine curriculum outlines the capabilities expected of a trainee participating in out of hours work in the different settings. There is no time-based requirement, but trainees need to evidence that they have met the curriculum capabilities.
The IM ARCP decision aid outlines the specific requirements for AUT.

